
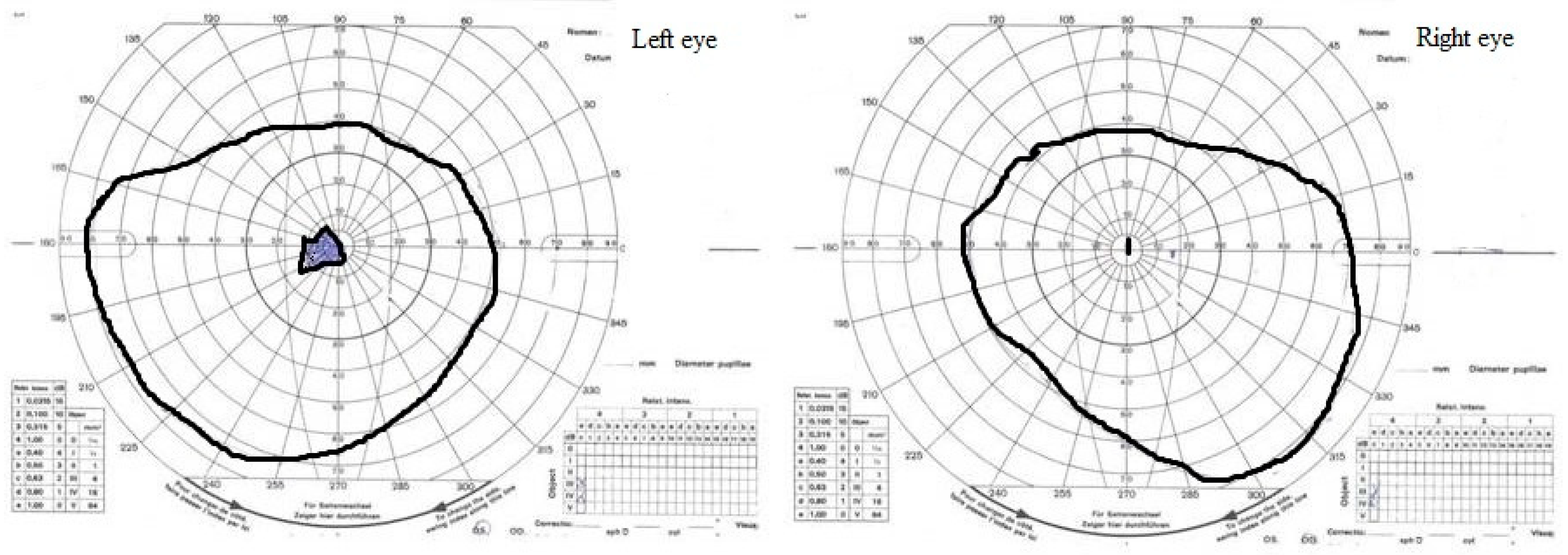
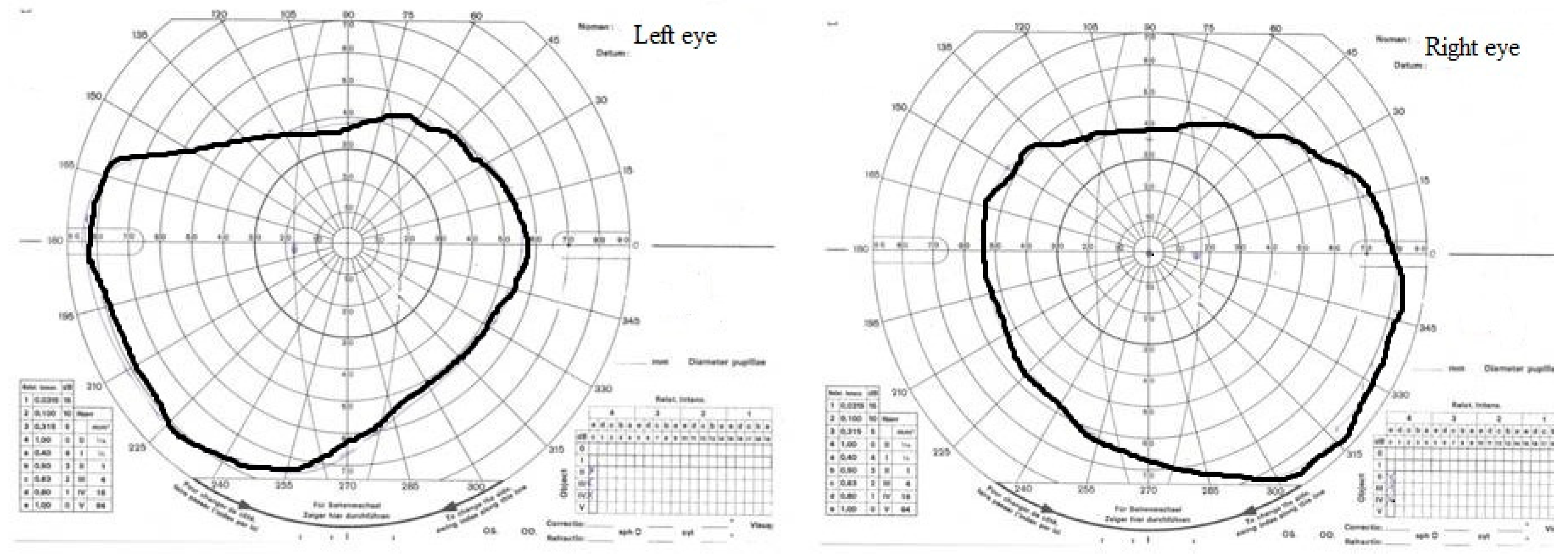
founded that the incidence of drusen is 10 times higher among members of the family with manifest optic nerve drusen. Genetically, optic nerve head drusen are inherited in autosomal dominant (AD) type of inheritance with variable penetration. The author also postulates the pathophysiological mechanisms of the formation and evolution of the drusen. A detailed structure was described by Tso in 1967. Clinically, they were described with the contribution of Liebreich in 1868, only 17 years after the construction of the direct ophthalmoscope. įor the first time, they were histologically recognized by Heinrich Muller in the nineteenth century (1858). They are less common in black people, equally represented among the sexes, while the average prevalence in the pediatric population is 0.4%. Their occurrence is most common in 3.4– adult white people (0.34–3.7%), with a frequent bilateral presentation in 75–85% of all cases. Thus, they are also considered to be one of the causes of the progressive type of optic neuropathy with genetic etiology. They are initially asymptomatic, but are not so rare and can cause lower visual acuity. This is a form of calcium degeneration of the axons of the optic nerve head (ONH). Optic nerve head drusen (ONHD) represent the congenital, developmental anomaly of the second cranial nerve. Neuroprotective drugs are investigated to reduce potential visual morbidity. After 6 months scotoma and loss of sensitivity of the visual field were reduced. The paper presents young female patient with bilateral optic nerve drusen and progressive visual field defects (scotomas), which implies topical hypotensive therapy. By reducing intraocular pressure, the compression to the optic nerve axons decreases, thus improving perfusion of the optic nerve head. Pilot studies confirmed benefit of topical hypotensive drugs even when drusen are not associated with glaucoma. Therapeutic procedures are medical, laser, and surgical. Useful diagnostic tools ophthalmoscopy, angiography, standard automated perimetry, B-scan ultrasonography, CT, OCT, HRT, GDx, and electrophysiological examination. Frequent complications: progressive visual field scotoma, ischemic optic neuropathy, central retinal artery or vein occlusion, and neovascularization adjacent to the optic nerve head. They are formed due to altered axonal transport, small diameter of scleral canal, direct compression, or ischemia. They are presented as acellular, hyaline deposits of globular appearance in front of the lamina cribrosa (prelaminar segment). They are initially asymptomatic but may causes progressive optic neuropathy.
Optic nerve head drusen (ONHD) represent congenital anomaly, which is a form of calcium degeneration of optic nerve head axons.


 0 kommentar(er)
0 kommentar(er)
